A3 – Development and characterization of artificial extracellular matrices based on collagen and glycosaminoglycan (GAG)-derivatives
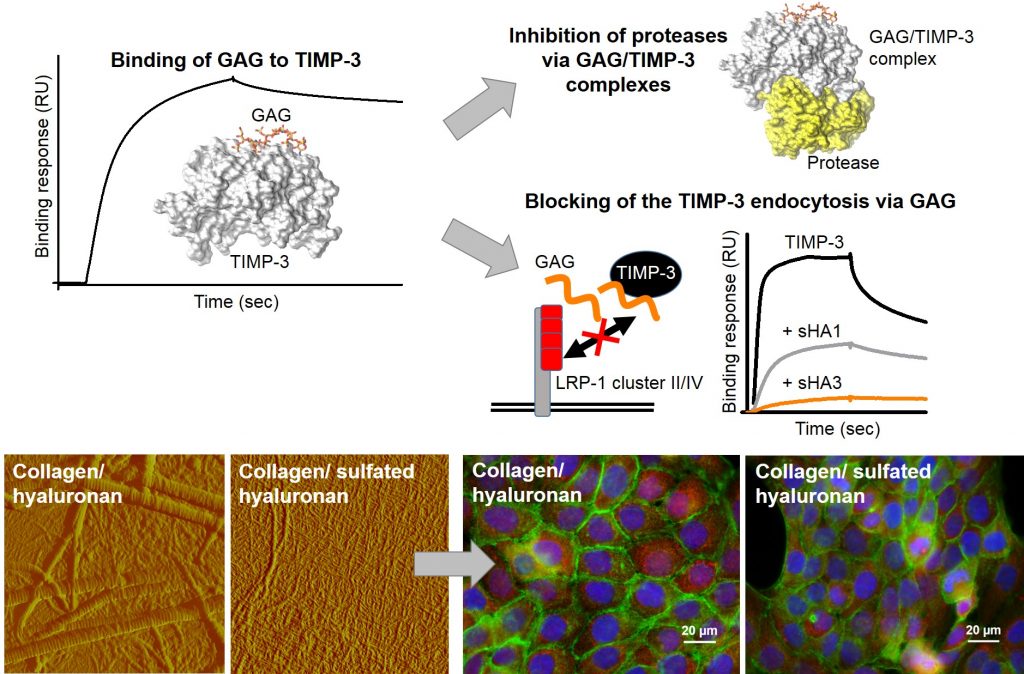
The demographical development with an increasing number of elderly, multimorbid patients has led to an accretive need for novel, functional biomaterials actively supporting tissue regeneration. The overall aim of this project A3 is to develop and characterize tissue-specific two- and three-dimensional artificial extracellular matrices (aECM). These aECM represent defined adjustable microenvironments to control cellular functions in bone and skin cells, e.g. by influencing mediator proteins (growth factors, interleukins) present during wound healing in vivo. Another focus of this project is to elucidate the structure-function relationship of glycosaminoglycan (GAG) derivatives in their interaction with mediator proteins relevant to healing processes. Biochemical and biophysical interaction analyses (e.g. surface plasmon resonance (SPR)) significantly contribute to an improved understanding of the molecular mechanisms by which GAG derivatives influence healing processes. Ultimately aECM with defined activity profiles should be available in particular for elderly, health-compromised patients.
Publications
- Balamurugan K, Koehler L, Dürig JN, Hempel U, Rademann J, Hintze V, Pisabarro MT. Structural insights into the modulation of PDGF/PDGFR-β complexation by hyaluronan derivatives. Biological Chemistry, vol. 402, no. 11, 2021, pp. 1441-1452. https://doi.org/10.1515/hsz-2021-0173.
- Schnabelrauch M, Schiller J, Möller S, Scharnweber D, Hintze V. Chemically modified glycosaminoglycan derivatives as building blocks for biomaterial coatings and hydrogels. Biological Chemistry, vol. 402, no. 11, 2021, pp. 1385-1395. https://doi.org/10.1515/hsz-2021-0171.
- Anderegg U, Halfter N, Schnabelrauch M, Hintze V. Collagen/glycosaminoglycan-based matrices for controlling skin cell responses. Biological Chemistry, vol. 402, no. 11, 2021, pp. 1325-1335. https://doi.org/10.1515/hsz-2021-0176.
- Al-Maawi S, Rother S, Halfter N, Fiebig KM, Moritz J, Moeller S, Schnabelrauch M, Kirkpatrick CJ, Sader R, Wiesmann HP, Scharnweber D, Hintze V, Ghanaati S. Covalent linkage of sulfated hyaluronan to the collagen scaffold Mucograft® enhances scaffold stability and reduces proinflammatory macrophage activation in vivo. Bioact. Mater. 2021, doi: 10.1016/ j.bioactmat.2021.06.008; shared senior authorship.
- Anderegg U, Halfter N, Schnabelrauch M, Hintze, V. Collagen/ glycosaminoglycan-based matrices for controlling skin cell responses. Biol. Chem. 2021, doi: 10.1515/hsz-2021-0176.
- Balamurugan K, Koehler L, Dürig J-N, Hempel U, Rademann J, Hintze V, Pisabarro MT. Structural insights into the modulation of PDGF/PDGFR-β complexation by hyaluronan derivatives. Biol Chem 2021, doi: 10.1515/hsz-2021-0173.
- Rother S, Ruiz-Gómez G, Koehler L, Balamurugan K, Fiebig KM, Galiazzo VD, Hempel U, Moeller S, Schnabelrauch M, Waltenberger J, Pisabarro MT, Scharnweber D, Hintze V. Hyaluronan/collagen hydrogels with sulfated glycosaminoglycans maintain VEGF165 activity and fine-tune endothelial cell response. ACS Appl. Bio Mater. 2021, 4, 1, 494–506.
- Schnabelrauch M, Schiller J, Möller S, Scharnweber D, Hintze V. Chemically modified glycosaminoglycan derivatives as building blocks for biomaterial coatings and hydrogels. Biol. Chem. 2021, doi: 10.1515/hsz-2021-0171.
- Gronbach M, Mitrach F, Möller S, Rother S, Friebe S, Mayr SG, Schnabelrauch M, Hintze V, Hacker MC, Schulz-Siegmund M. A versatile macromer-based glycosaminoglycan (sHA3) decorated biomaterial for pro-osteogenic scavenging of Wnt antagonists. Pharmaceutics 2020, 12(11):1037.
- Hauck S, Zager P Halfter N, Wandel E, Torregrossa M, Kakpenova A, Rother S, Ordieres M, Räthel S, Berg A, Möller S, Schnabelrauch M, Simon JC, Hintze V, Franz S. Collagen/hyaluronan based hydrogels releasing sulfated hyaluronan improve dermal wound healing in diabetic mice via reducing inflammatory macrophage activity. Bioactive Materials 2021, 6, 4342–4359.DOI: 10.1016/j.bioactmat.2021.04.026.
- Förster Y, Schulze S, Penk A, Neuber C, Möller S, Hintze V, Scharnweber D, Schnabelrauch M, Pietzsch J, Huster D, Rammelt S. The influence of different artificial extracellular matrix implant coatings on the regeneration of a critical size femur defect in rats. Mater Sci Eng C Mater Biol Appl. 2020, 116:111157.
- Gronbach M, Mitrach F, Lidzba V, Müller B, Möller S, Rother S, Salbach-Hirsch J, Hofbauer LC, Schnabelrauch M, Hintze V, Hacker MC, Schulz-Siegmund M. Scavenging of Dickkopf-1 by macromer-based biomaterials covalently decorated with sulfated hyaluronan displays pro-osteogenic effects. Acta Biomater. 2020 Sep 15;114:76-89. doi: 10.1016/j.actbio.2020.07.017. Epub 2020 Jul 13. PMID: 32673749.
- Koehler L, Ruiz-Gómez G, Balamurugan K, Rother S, Freyse J, Möller S, Schnabelrauch M, Köhling S, Djordjevic S, Scharnweber D, Rademann J, Pisabarro MT, Hintze V. Dual Action of Sulfated Hyaluronan on Angiogenic Processes in Relation to Vascular Endothelial Growth Factor-A. Sci Rep. 2019 Dec 2;9(1):18143. doi: 10.1038/s41598-019-54211-0.
- Lee PS, Hess R, Friedrichs J, Haenchen V, Eckert H, Cuniberti G, Rancourt D, Krawetz R, Hintze V, Gelinsky M, Scharnweber D. Recapitulating bone development events in a customised bioreactor through interplay of oxygen tension, medium pH, and systematic differentiation approaches. J Tissue Eng Regen Med. 2019 Sep;13(9):1672-1684. doi: 10.1002/term.2921. Epub 2019 Jul 15.
- Rother S, Krönert V, Hauck N, Berg A, Moeller S, Schnabelrauch M, Thiele J, Scharnweber D, Hintze V. Hyaluronan/collagen hydrogel matrices containing high-sulfated hyaluronan microgels for regulating transforming growth factor-β1. J Mater Sci Mater Med. 2019 May 24;30(6):65. doi: 10.1007/s10856-019-6267-1.
- Schneider M, Rother S, Möller S, Schnabelrauch M, Scharnweber D, Simon JC, Hintze V, Savkovic V. Sulfated hyaluronan-containing artificial extracellular matrices promote proliferation of keratinocytes and melanotic phenotype of melanocytes from the outer root sheath of hair follicles. J Biomed Mater Res A. 2019 Aug;107(8):1640-1653. doi: 10.1002/jbm.a.36680. Epub 2019 Apr 23.
- Wojak-Ćwik IM, Rumian Ł, Krok-Borkowicz M, Hess R, Bernhardt R, Dobrzyński P, Möller S, Schnabelrauch M, Hintze V, Scharnweber D, Pamuła E. Synergistic effect of bimodal pore distribution and artificial extracellular matrices in polymeric scaffolds on osteogenic differentiation of human mesenchymal stem cells. Mater Sci Eng C Mater Biol Appl. 2019 Apr;97:12-22. doi: 10.1016/j.msec.2018.12.012. Epub 2018 Dec 7.
- Kratochvil I, Hofmann T, Rother S, Schlichting R, Moretti R, Scharnweber D, Hintze V, Escher BI, Meiler J, Kalkhof S, von Bergen M. Mono(2-ethylhexyl) phthalate (MEHP) and mono(2-ethyl-5-oxohexyl) phthalate (MEOHP) but not di(2-ethylhexyl) phthalate (DEHP) bind productively to the peroxisome proliferator-activated receptor γ. Rapid Commun Mass Spectrom. 2019 May;33 Suppl 1:75-85. doi: 10.1002/rcm.8258. Epub 2019 Jan 1.
- Krieghoff J, Picke AK, Salbach-Hirsch J, Rother S, Heinemann C, Bernhardt R, Kascholke C, Möller S, Rauner M, Schnabelrauch M, Hintze V, Scharnweber D, Schulz-Siegmund M, Hacker MC, Hofbauer LC, Hofbauer C. Increased pore size of scaffolds improves coating efficiency with sulfated hyaluronan and mineralization capacity of osteoblasts. Biomater Res. 2019; 23:26. doi: 10.1186/s40824-019-0172-z.
- Neuber C, Schulze S, Förster Y, Hofheinz F, Wodke J, Möller S, Schnabelrauch M, Hintze V, Scharnweber D, Rammelt S, Pietzsch J. Biomaterials in repairing rat femoral defects: In vivo insights from small animal positron emission tomography/computed tomography (PET/CT) studies. Clin Hemorheol Microcirc. 2019; 73:177-194. doi: 10.3233/CH-199208.
- Rauner M, Baschant U, Roetto A, Pellegrino RM, Rother S, Salbach-Hirsch J, Weidner H, Hintze V, Campbell G, Petzold A, Lemaitre R, Henry I, Bellido T, Theurl I, Altamura S, Colucci S, Muckenthaler MU, Schett G, Komla-Ebri DSK, Bassett JHD, Williams GR, Platzbecker U, Hofbauer LC. Transferrin receptor 2 controls bone mass and pathological bone formation via BMP and Wnt signaling. Nature Metabolism. 2019; 1:111–24.
- Thönes S, Rother S, Wippold T, Blaszkiewicz J, Balamurugan K, Moeller S, Ruiz-Gómez G, Schnabelrauch M, Scharnweber D, Saalbach A, Rademann J, Pisabarro MT, Hintze V, Anderegg U. Hyaluronan/collagen hydrogels containing sulfated hyaluronan improve wound healing by sustained release of heparin-binding EGF-like growth factor. Acta Biomater. 2019; 86:135-147.
- Corsuto L, Rother S, Koehler L, Bedini E, Moeller S, Schnabelrauch M, Hintze V, Schiraldi C, Scharnweber D. Sulfation degree not origin of chondroitin sulfate derivatives modulates keratinocyte response. Carbohydr Polym. 2018, 191:53-64.
- Nordsieck K, Baumann L, Hintze V, Pisabarro MT, Schnabelrauch M, Beck-Sickinger AG, Samsonov SA. The effect of interleukin-8 truncations on its interactions with glycosaminoglycans. Biopolymers 2018, doi: 10.1002/bip.23103.
- Rother S, Galiazzo V, Kilian D, Fiebig KM, Becher J, Moeller S, Schnabelrauch M, Waltenberger J, Hintze V and Scharnweber D. Hyaluronan/collagen hydrogels with sulfated hyaluronan for improved repair of vascularized tissue tune the binding of proteins and promote endothelial cell growth. Macromolecular Bioscience. 2017. [Epub ahead of print]
- Bhowmick S, Rother S, Zimmermann H, Lee PS, Moeller S, Schnabelrauch M, Koul V, Jordan R, Hintze V, Scharnweber D. Biomimetic electrospun scaffolds from main extracellular matrix components for skin tissue engineering application – The role of chondroitin sulfate and sulfated hyaluronan. Mater Sci Eng C Mater Biol Appl. 2017; 79:15-22.
- Koehler L, Samsonov S, Rother S, Vogel S, Köhling S, Moeller S, Schnabelrauch M, Rademann J, Hempel U, Pisabarro MT, Scharnweber D, Hintze V. Sulfated Hyaluronan Derivatives Modulate TGF-ß1:Receptor Complex Formation: Possible Consequences for TGF-ß1 Signaling. Sci Rep. 2017; 7:1210.
- Rother S, Samsonov SA, Moeller S, Schnabelrauch M, Rademann J, Blaszkiewicz J, Köhling S, Waltenberger J, Pisabarro MT, Scharnweber D, Hintze V. Sulfated Hyaluronan Alters Endothelial Cell Activation in Vitro by Controlling the Biological Activity of the Angiogenic Factors Vascular Endothelial Growth Factor-A and Tissue Inhibitor of Metalloproteinase-3. ACS Appl Mater Interfaces. 2017; 9:9539-9550.
- Metzger W, Rother S, Pohlemann T, Möller S, Schnabelrauch M, Hintze V, Scharnweber D. Evaluation of cell-surface interaction using a 3D spheroid cell culture model on artificial extracellular matrices. Mater Sci Eng C Mater Biol Appl. 2017; 73:310-318.
- Förster Y, Bernhardt R, Hintze V, Möller S, Schnabelrauch M, Scharnweber D, Rammelt S. Collagen/glycosaminoglycan coatings enhance new bone formation in a critical size bone defect – A pilot study in rats. Mater Sci Eng C Mater Biol Appl. 2017; 71:84-92.
- Rother S, Samsonov SA, Hofmann T, Blaszkiewicz J, Köhling S, Moeller S, Schnabelrauch M, Rademann J, Kalkhof S, von Bergen M, Pisabarro MT, Scharnweber D, Hintze V. Structural and functional insights into the interaction of sulfated glycosaminoglycans with tissue inhibitor of metalloproteinase-3 – a possible regulatory role on extracellular matrix homeostasis. Acta Biomater. 2016;45:143-154.
- Rother S, Samsonov SA, Hempel U, Vogel S, Moeller S, Blaszkiewicz J, Köhling S, Schnabelrauch M, Rademann J, Pisabarro MT, Hintze V, Scharnweber D. Sulfated hyaluronan alters the interaction profile of TIMP-3 with the endocytic receptor LRP-1 cluster II and IV and increas-es the extracellular TIMP-3 level of human bone marrow stromal cells. Biomacromolecules. 2016;17:3252-61.
- Picke AK, Salbach-Hirsch J, Hintze V, Rother S, Rauner M, Kascholke C, Möller S, Bernhardt R, Rammelt S, Pisabarro MT, Ruiz-Gómez G, Schnabelrauch M, Schulz-Siegmund M, Hacker MC, Scharnweber D, Hofbauer C, Hofbauer LC. Sulfated hyaluronan improves bone regeneration of diabetic rats by binding sclerostin and enhancing osteoblast function. Biomaterials. 2016;96:11-23.
- Salbach-Hirsch J, Samsonov SA, Hintze V, Hofbauer C, Picke AK, Rauner M, Gehrcke JP, Moeller S, Schnabelrauch M, Scharnweber D, Pisabarro MT, Hofbauer LC. Structural and func-tional insights into sclerostin-glycosaminoglycan interactions in bone. Biomaterials. 2015;67:335-45.
- Rother S, Salbach-Hirsch J, Moeller S, Seemann T, Schnabelrauch M, Hofbauer LC, Hintze V, Scharnweber D. Bioinspired collagen/glycosaminoglycan-based cellular microenvironments for tuning osteoclastogenesis. ACS Appl Mater Interfaces. 2015;7:23787-97.
- Miron A, Rother S, Huebner L, Hempel U, Käppler I, Moeller I, Schnabelrauch M, Scharnweber D ,Hintze V. Sulfated Hyaluronan Influences the Formation of Artificial Extracellular Matrices and the Adhesion of Osteogenic Cells. Macromolecular Bioscience, 2014;14:1783-94.
- Hintze V, Samsonov SA, Anselmi M, Moeller S, Becher J, Schnabelrauch M, Scharnweber D, Pisabarro MT. Sulfated Glycosaminoglycans Exploit the Conformational Plasticity of Bone Morphogenetic Protein-2 (BMP-2) and Alter the Interaction Profile with Its Receptor. Biomacromolecules 2014; 15 (8): 3083-92.
- Hempel U, Preissler C, Vogel S, Möller S, Hintze V, Becher J, Schnabelrauch M, Rauner M, Hofbauer LC, Dieter P. Artificial Extracellular Matrices with Oversulfated Glycosaminoglycan Derivatives Promote the Differentiation of Osteoblast-Precursor Cells and Premature Osteoblasts. BioMed Research International 2014, DOI 10.1155/2014/93;8368.
- Hempel U, Matthäus C, Preissler C, Möller S, Hintze V, Dieter P., Artificial matrices with high-sulfated glycosaminoglycans and collagen are anti-inflammatory and pro-osteogenic for human mesenchymal stromal cells. J Cell Biochem. 2014; 115 (9): 1561-71.
- Salbach-Hirsch J, Ziegler N, Thiele S, Moeller S, Schnabelrauch M, Hintze V, Scharnweber D, Rauner M, Hofbauer LC. Sulfated Glycosaminoglycans Support Osteoblast Functions and Concurrently Suppress Osteoclasts. J Cell Biochem. 2014; 115 (6): 1101-11.
- Förster Y, Hintze V, Rentsch C, Rentsch B, Bierbaum S, Wiesmann HP, Scharnweber D, Worch H,Rammelt S. Surface functionalization of biomaterials with tissue-inductive artificial extracellular matrices. BioNanoMat 2013; 14 (3-4): 143–152.
- De Barros RRM, Novaes AB, Korn P, Queiroz A, de Almeida ALG, Hintze V, Scharnweber D, Bierbaum S, Stadlinger. Bone formation in a local defect around dental implants coated with extracellular matrix components. Clin Implant Dent Relat Res 2013,17:742-57.
- Schulz MC, Korn P, Stadlinger B, Range U, Moeller S, Becher J, Schnabelrauch M, Mai, R, Scharnweber D, Eckelt U, Hintze V. Coating with artificial matrices from collagen and sulfated hyaluronan influences the osseointegration of dental implants. J Mater Sci Mater Med. 2014; 25 (1): 247-258.
- Korn P, Schulz MC, Hintze V, Range U, Mai R, Eckelt U, Schnabelrauch M, Möller S, Becher J, Scharnweber D, Stadlinger B. Chondroitin sulfate and sulfated hyaluronan containing collagen coatings of titanium implants influence peri-implant bone formation in a minipig model. J Biomed Mater Res A. 2014; 102 (7): 2334-44.
- Salbach-Hirsch J, Kraemer J, Rauner M, Samsonov SA, Pisabarro MT, Moeller S, Schnabelrauch M, Scharnweber D, Hofbauer LC, Hintze V.
- The promotion of osteoclastogenesis by sulfated hyaluronan through interference with osteoprotegerin and receptor activator of NF-?B ligand/osteoprotegerin complex formation. Biomaterials 2013, 34:7653-7661.
- van der Smissen A, Samsonov S, Hintze V, Scharnweber D, Moeller S, Schnabelrauch M, Pisabarro MT, Anderegg U. Artificial extracellular matrix composed of collagen I and highly sulfated hyaluronan interferes with TGF?(1) signaling and prevents TGF?(1)-induced myofibroblast differentiation. Acta Biomater. 2013, 9: 7775–7786.
- Wojak-Cwik IM, Hintze V, Schnabelrauch M, Moeller S, Dobrzynski P, Pamula E, Scharnweber D. Poly(L-lactide-co-glycolide) scaffolds coated with collagen and glycosaminoglycans: mpact on proliferation and osteogenic differentiation of human mesenchymal stem cells. J Biomedical Mater Res A. 2013, 101(11):3109-22.
- Hess R, Jeschnke A, Neubert H, Hintze V, Moeller S, Schnabelrauch M, Wiesmann HP, Hart DA, Scharnweber D. Synergistic effect of defined artificial extracellular matrices and pulsed electric fields on osteogenic differentiation of human MSCs. Biomaterials. 2012;33:8975-85.
- Bierbaum S, Hintze V, Scharnweber D. Functionalization of biomaterials surfaces using artificial extracellular matrices. Biomatter. 2012;2:132-41.
- Hempel U, Möller S, Noack C, Hintze V, Scharnweber S, Schnabelrauch M, Dieter P. Sulfated hyaluronan/collagen I-matrices enhance osteogenic differentiation of human mesenchymal stromal cells in vitro even in the absence of dexamethasone. Acta Biomater. 2012;8:4064-72.
- Hintze V, Miron A, Möller S, Schnabelrauch M, Heinemann S, Worch H, Scharnweber D. Artificial extracellular matrices of collagen and sulfated hyaluronan enhance the differentiation of human mesenchymal stem cells in the presence of dexamethasone. J Tissue Eng Regen Med. 2012;doi 10.1k02/term.1528.
- Hempel U, Hintze V, Möller S, Schnabelrauch M, Scharnweber D, Dieter P. Artifical extracellular matrices composed of collagenI and sulfated hyaluronan with adsorbed transforming growth factor ?-1 promote collagen synthesis of human mesenchymal stromal cells. Acta Biomater. 2012;8:659-66.
- Becher J, Möller S, Riemer T, Schiller J, Hintze V, Bierbaum S, Scharnweber D, Worch H, Schnabelrauch M. Sulfated glycosaminoglycan building blocks for the design of artificial extracellular matrices. Book chapter in: ACS Symposium Series. 2012;1107:315-28.
- Bierbaum S, Hintze V, Scharnweber D. Functionalization of biomaterials surfaces using artificial extracellular matrices. Biomatter. 2012;2:132-41.
- Stadlinger B, Hintze V, Bierbaum S, Möller S, Schulz MC, Maia R, Heinemann S, Scharnweber D, Schnabelrauch M, Eckelt U. Biological functionalization of dental implants with collagen and glycosaminoglycans – a comparative study. J Biomed Mater Res B Appl Biomater. 2012;100:331-41.
- Franz S, Forstreuter I, Hintze V, Möller S, Scharnweber D, Schnabelrauch M, Simon JC. Immunomodulatory effects on dendritic cells of biomaterial coatings based on artificial extracellular matrices (aECM). Experimental Dermatology. 2011;20:182.
- van der Smissen A, Hintze V, Scharnweber D, Moeller S, Schnabelrauch M, Majok A, Simon JC, Anderegg U. Growth promoting substrates for human dermal fibroblasts provided by artifical extracellular matrices composed of collagen I and sulfated glycosaminoglycans. Biomaterials. 2011;32:8938-46.
- Campbell GM, Bernhardt R, Scharnweber D, Boyd SK. The bone architecture is enhanced with combined PTH and alendronate treatment compared to monotherapy while maintaining the state of surface mineralization in the OVX rat. Bone. 2011;49:225-32.
- Franz S, Rammelt S, Scharnweber D, Simon JC. Immune responses to implants – A review of the implications for the design of immunomodulatory biomaterials. Biomaterials. 2011;32:6692-709.
- Hintze V, Moeller S, Schnabelrauch M, Bierbaum S, Viola M, Worch H, Scharnweber D. Modifications of Hyaluronan Influence the Interaction with Human Bone Morphogenetic Protein-4 (hBMP-4). Biomacromolecules. 2009;10:3290-3297.
- Wojak I, Pamula E, Dobrzynski P, Zimmermann H, Worch H, Scharnweber D, Hintze V. Coating of poly(L-actide-co-glycolide) scaffolds with collagen /glycosaminoglycan matrices and their effect on osteoblast behaviour. Engineering of Biomaterials. 2009;86:9-13.
- Stadlinger B, Pilling E, Huhle M, Mai R, Bierbaum S, Scharnweber D, Kuhlisch E, Loukota R, Eckelt U. Evaluation of osseointegration of dental implants coated with collagen, chondroitin sulphate and BMP-4: an animal study. Int J Oral Maxillofac Surg. 2008;37:54-9.
- Douglas T, Hempel U, Mietrach C, Viola M, Vigetti D, Heinemann S, Bierbaum S, Scharnweber D, Worch H. Influence of collagen-fibril-based coatings containing decorin and biglycan on osteoblast behavior. J Biomed Mater Res A 2008;84:805-16.
- Stadlinger B, Pilling E, Mai R, Bierbaum S, Berhardt R, Scharnweber D, Eckelt U. Effect of biological implant surface coatings on bone formation, applying collagen, proteoglycans, glycosaminoglycans and growth factors. J Mater Sci Mater Med. 2008;19:1043-9.
- Douglas T, Heinemann S, Mietrach C, Hempel U, Bierbaum S, Scharnweber D, Worch H. Interactions of Collagen Types I and II with Chondroitin Sulfates A-C and Their Effect on Osteoblast Adhesion. Biomacromolecules 2007;8:1085-92.
- Bierbaum S, Douglas T, Hanke T, Scharnweber D, Tippelt S, Monsees TK, Funk RH, Worch H. Collageneous matrix coatings on titanium implants modified with decorin and chondroitin sulfate: characterization and influence on osteoblastic cells. J Biomed Mater Res A. 2006;77:551-62.
- Bierbaum S, Beutner R, Hanke T, Scharnweber D, Hempel U, Worch H. Modification of Ti6Al4V surfaces using collagen I, III and fibronectin. I. Biochemical and morphological characteristics of the adsorbed matrix. J Biomed Mater Res A. 2003;67:421-30.
Contact

PD Dr. rer.nat. Vera Hintze
Research Assistant and Research Group Leader
Dresden University of Technology
Faculty of Mechanical Engineering
Max Bergmann Center for Biomaterials
Budapester Straße 27, 01062 Dresden
Phone: +49 (0)351 – 463 39389
E-Mail: Vera.Hintze@tu-dresden.de
Web: https://tu-dresden.de/ing/maschinenwesen/ifww/biomaterialien/forschung/funktionelle-biomaterialien
